Faculty Spotlight: Natalie Voigt on Using Case-Based Learning to Increase Student Critical Thinking in Nursing Education

Natalie Voigt is an Assistant Professor of Nursing in the Masters Direct Entry Nursing program at CUIMC. The MDE program is a rigorous 15 month accelerated graduate nursing program that recruits students from various undergraduate and professional backgrounds. Dr. Voigt was awarded an Office of the Provost Innovative Course Module Design Grant for her course “The Science of Nursing Practice with Adults II,” which is one of two medical surgical nursing courses offered in the program. Below, Dr. Voigt discusses the innovations she made with the support of the Center for Teaching and Learning in her funded project titled “Increasing Student Critical Thinking Through Case-Based Learning Modules in Medical Surgical Nursing Education.”
Please describe the previous iteration of the curriculum and its main challenges/limitations.
The central objective of our nursing curriculum is to cultivate critical thinking skills necessary for sound clinical reasoning and clinical decision making to be safe and competent nurses. However, it seemed as though in my experience, there were inconsistencies among the students’ ability to demonstrate adequate critical thinking related to clinical decision making in the classroom and clinical areas.
Evidence suggests that students instructed using case-based learning compared to students taught using lecture-based learning show significant improvements—not only in critical thinking ability, but also in communication and self-directed learning skills necessary for lifelong successful nursing practice. This led me to conclude that my static PowerPoint presentations may not be the most effective tool. So, the purpose of this grant was to receive support to create case-based learning modules that would engage students in more active learning processes to enhance critical thinking skills necessary for safe and competent nursing practice.
What is the intervention that you implemented and how does it enhance the student learning experience?
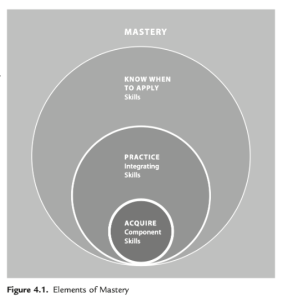
The pedagogical underpinnings of my project centered on the Elements of Mastery model by Ambrose (figure 4.1). This nested model describes the criteria to be met in order for mastery to be achieved in any discipline. At the foundational level, students acquire basic knowledge and skills necessary for nursing practice obtained from my pre-recorded lecture content, reading the text, and watching demonstrations of skills videos. Only after knowledge and skills are attained, can integration commence through practice. It is during this next stage of practice where case studies would be used to reinforce the knowledge and skills obtained. Application of this knowledge would be further reinforced in the simulation lab and clinical setting, which would allow for more integrated hierarchical scaffolding of education beyond just simple identification of appropriate interventions for patients.
The interventions implemented as part of this redesign included a creation of pre-recorded lecture content, which was made available to the students to review asynchronously, the creation of evolving case studies for in-person small group discussions, and completion facilitated by the professor and the TAs. At the conclusion of the case, a debrief was created along with opportunities for individual self-reflection using a two-question ungraded quiz. Evaluation of case-based learning was achieved through weekly ungraded quizzes, our course evaluations, and student testimony.
Can you provide an example from your course?
Below is an example of an evolving case used during our hematology unit. This case centers on a patient with a history of sickle cell disease and each case employs different levels of questions based on Bloom’s taxonomy.
At the start of every case, the first set of questions query the students’ remembering and understanding—recalling basic facts and concepts, and explaining ideas. Then the case will evolve with a change in the patient status. Subsequent questions challenge the students to shift their priorities in some way—is there a complication that’s evolving that requires more attention than the initial priority? Do they need to contact a provider? And what evidence do they have that supports that need to contact the provider? Do they need to call a rapid response or a code, etc.? This employs application, or even analyzing other questions. Then finally, the case concludes with some psychosocial aspect. In this case, addressing misconceptions of the patient’s pain response based on historical race-based medicine, in which I ask the students to evaluate and respond to the following patient’s statement, “One of my biggest fears is that I’ll come in here in crisis and the doctor won’t treat my pain aggressively enough. I don’t want to be labeled as a drug seeker or an emergency room abuser.” In other cases, we explore end of life decisions and discussions with family members, and in others, family dynamics and patient-centered care. In this part of the case, students have to identify their positions in these often difficult, but real life examples of care and thereby have the opportunity to employ evaluation-level questions.
| V.M. is a 29-year-old African American client with a history of sickle cell disease (SCD) marked by frequent episodes of severe pain. His anemia has been managed with multiple transfusions. Six months ago, he started showing signs of chronic renal failure. His regular medications are oxycodone-acetaminophen (Percocet), hydroxyurea (Droxia), and folic acid. In the hematology clinic this morning, V.M.’s hemoglobin measured 6.7 g/dL. He received 2 units of packed red blood cells (PRBCs) over 3 hours/unit and then went home. He developed dyspnea and shortness of breath approximately 2 hours later, and his wife called 911. The EMTs initiated oxygen at 8 L per nasal cannula and transported V.M. to the ED.
When V.M. arrives at the ED, you perform a quick assessment and note crackles in V.M.’s bases bilaterally. Vital signs are 176/102, 94, 28, 97.8 ° F (36.6 ° C), and Spo2 78%. Peripheral pulses are equal and 3+. Acting according to the standing orders for your institution, you start an IV line and draw blood for a CBC with differential and a BMP.
The physician prescribes furosemide (Lasix) 40 mg IV push (IVP) now. V.M. voids 1900 mL within 2 hours of the furosemide (Lasix) administration. As V.M.’s dyspnea is relieved, he shakes the physician’s hand and thanks them for asking about the presence of pain and the need for pain medication. V.M. states, “One of my biggest fears is that I’ll come in here in crisis and the doctor won’t treat my pain aggressively enough. I don’t want to be labeled as a drug seeker or an emergency room abuser.”
|
What were the results?
This is a summary of my course evaluation ratings on two particular items I was focused on improving, especially as a new educator: “The materials were presented in a logical, organized manner” and “Important content was clearly and understandably communicated.” My course is taught every five weeks over the fall and spring semesters, which explains the five data points. This chart demonstrates rotations one, two, three, four and five during the year of my first year of teaching prior to the grant, and then data points following the grant and the support I received. When I plugged these values into a simple t-test, the difference between my first year of teaching, and my second year of teaching with CTL support through my Provost award showed a significant improvement.
| Survey Item | Pre Grant Data | Post Grant Data | P-value |
| The materials were presented in a logical, organized manner. |
3.75 3.40 |
4.83 4.65 4.44 4.23 4.66 |
.043 |
| Important content was clearly and understandably communicated. | 3.33 2.80 2.29 4.27 4.00 |
4.78 4.53 4.26 4.16 4.63 |
.042 |
Student testimonials
Student testimonials were also very important in my evaluation of the implementation of the CDL modules. Below are some of the students’ responses. Besides the objectives of increasing critical thinking, it was important to me to build a learning community in my classroom and create more of a student-instructor partnership in their education, and I hope I achieved that.
“Participating in the case study group is a great opportunity to apply lecture knowledge and helps reinforce your understanding and comfort level with the material.”
“This is a safe space to make mistakes and ask as many questions as possible. It is helpful to delegate questions between group members for the sake of time management. Utilize your TAs, they are here to help you!”
“Don’t be too hard on yourself, you may feel uncomfortable and anxious at first, but you will get better. And use each other to answer questions, ‘teamwork makes the dream work.’ Remember that you know more than you think and don’t second guess yourself.”
This spotlight is a condensed version of Natalie’s video presentation at the 2022 Celebration of Teaching and Learning Symposium.